 Junior was presented to our Oncology service for consultation following a diagnosis of cutaneous hemangiosarcoma made via biopsy of a mass removed by his primary care veterinarian. The mass had been present for about 4 months and started to grow rapidly leading up to its removal. Histopathology of the mass was most consistent with a diagnosis of cutaneous hemangiosarcoma. Unfortunately, invasion into subcutaneous tissue was observed and complete excision could not be confirmed. Both variables have been associated with an unfavorable prognosis.
Junior was presented to our Oncology service for consultation following a diagnosis of cutaneous hemangiosarcoma made via biopsy of a mass removed by his primary care veterinarian. The mass had been present for about 4 months and started to grow rapidly leading up to its removal. Histopathology of the mass was most consistent with a diagnosis of cutaneous hemangiosarcoma. Unfortunately, invasion into subcutaneous tissue was observed and complete excision could not be confirmed. Both variables have been associated with an unfavorable prognosis.
On examination, Junior had a few other cutaneous and subcutaneous masses, one of which had some bruising resembling a second cutaneous hemangiosarcoma. Junior was staged completely with chest X-rays and an abdominal ultrasound, which did not reveal any evidence of metastasis. Since Junior was at a higher risk for local tumor recurrence and metastasis, treatment with chemotherapy was indicated in his case. Treatment options offered to the client included additional surgery to obtain wider margins, injectable doxorubicin therapy and/or metronomic chemotherapy, which involves continuous administration of low-dose oral chemotherapy.
The owner elected to move forward with metronomic chemotherapy as this option has been associated with fewer side effects. Approximately 5 months after initiating therapy, Junior’s cancer progressed in the form of multiple new cutaneous masses and pulmonary metastasis (Image). Vorinostat, an alternative oral chemotherapy drug, was added to Junior’s treatment regimen at that time due to apparent synergistic antiangiogenic effects with metronomic chemotherapy. Vorinostat is histone deacetylase (HDAC) inhibitor, which allows for activation of genes involved in cell cycle arrest resulting in tumor cell death.
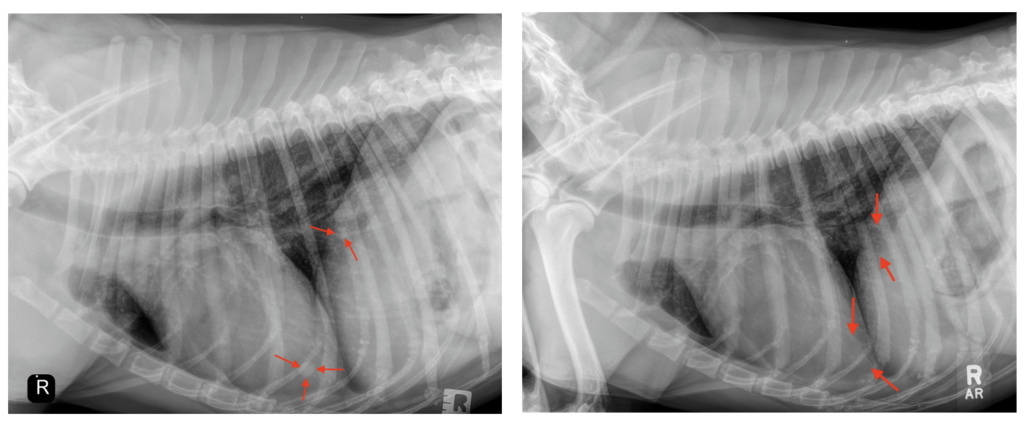
Thoracic radiographs taken in April (LEFT) revealed evidence of soft tissue nodules (arrows) consistent with pulmonary metastasis. Repeat radiographs performed in July (RIGHT) to assess Junior’s response to combination therapy revealed complete resolution of the previously noted nodules (arrows).
Approximately 3 months after initiating combination therapy, Junior presented to PVESC for restaging to assess his response to treatment. On examination, ALL of Junior’s previously noted cutaneous and subcutaneous masses had completely resolved and chest X-rays revealed complete resolution of all pulmonary nodules (Image). Continued treatment with combination therapy until either cancer progression or toxicity was recommended at that time. The PVESC Oncology team feels honored to have been a part in Junior’s cancer journey.
CLINICALLY RELEVANT FACTS:
- Cutaneous hemangiosarcoma typically carries an excellent prognosis following complete surgical excision.
- Invasion into the subcutaneous tissue and incomplete excision may significantly impact overall prognosis as in Junior’s case. Thus, complete tumor removal with wide margins is vital to improving long-term outcome.
- Novel approaches to cancer management with targeted therapies, such as Vorinostat, have improved our ability to successfully manage cancer patients with advanced disease.
Authored by: Dr. Brittanie Partridge, DMV, PhD, DACVIM, Oncology